Celiac disease is only one of several gluten-related disorders. A recent paradigm shift has occurred within the healthcare field with the recognition that non-celiac gluten sensitivity is at least six-fold, and (so far) as high as 20-fold more frequent than celiac disease — and there are even more gluten-related disorders where those came from.
How do we differentiate the world of gluten-related disorders? This is a critical discussion. Would you treat an IgE reaction the same as an IgA reaction? There are similarities in protocols, but each carries a different emphasis.
There is a spectrum of gluten-related disorders. Now, what does that mean? It means there are at least four different conditions that fall under the category of a “gluten-related disorder.”
Here we cover the four most recognized categories of gluten-related disorders.
Allergy (IgE)
The first one—the oldest of these in terms of being identified in medical literature—is an allergy, more specifically a wheat allergy. That’s an IgE reaction. And those tests came out in the 1950s. The skin prick test is still used today. It can be diagnosed by skin pricking or by a blood test.
Any other immunoglobulin response cannot be called an allergy because the first immune response that was identified was coined as an allergy — an IgE response.
To get your language right so that you are referring to the proper conditions when you’re talking with your peers, do not refer to a gluten-related disorder as an allergy unless there is an IgE response present. Refer to it simply as a gluten-related disorder.
Common symptoms of a wheat allergy include:
- Swelling, itching or irritation of the mouth or throat
- Hives, itchy rash or swelling of the skin
- Stuffy or runny nose
- Headaches
- Itchy, watery eyes
- Cramps, nausea or vomiting
- Diarrhea
In the following serious but rare circumstances listed below, seek emergency treatment immediately:
- Difficulty breathing
- Anaphylaxis
- Heart palpitations
Celiac Disease
Celiac disease is the most well-known gluten-related disorder. In fact, many people don’t even realize there are other gluten-related problems other than celiac disease. It’s an autoimmune condition that results in tissue damage in the small intestine. Celiac disease is unique and separate in its own way.
The standard test for celiac disease looks at transglutaminase antibodies [IgA transglutaminase antibodies]. There are nine different transglutaminases. We look at transglutaminase 2, which is on the microvilli in the intestines. It also covers the organs, liver, kidneys, heart, and spleen.
This test is considered the diagnostic marker for celiac disease, but there’s a problem with the test. It shows transglutaminase ninety-seven percent sensitive to identify celiac disease.
The problem is that the researchers use celiac patients in these studies, and to qualify as a celiac patient, you have total villous atrophy. In order to get diagnosed, a patient would have had an endoscopy where a doctor could see that the microvilli were worn down completely. So, if you have total villous atrophy, the transglutaminase blood test will be accurate 9.5 to 9.9 out of 10 times.
But, if you have partial villous atrophy, the test may come back negative — that’s a problem. You won’t see it in that blood test because it’s only sensitive at total villous atrophy.
I would personally like to change how the medical community views and tests for celiac disease. Rather than wait until you have reached the final stage, I propose we look at it as a spectrum so people can identify the problem early on and follow a gluten-free protocol.
We already have the ability to do this. In the US, we have an excellent tool to distinguish between celiac, non-celiac gluten sensitivity, non-gluten wheat sensitivity and autoimmune processes triggered by gluten: the Vibrant Wellness Wheat Zoomer test. At this time, it is available everywhere in the US except New York.
Cyrex Array Panels are available both the US and internationally.
Unless you notice an immediate reaction upon eating a food, it can be difficult to make the association between the food and symptoms that can appear later. Many people with celiac experience problems outside of their gut, making it even less likely to make a food association.
Some Common Symptoms of Celiac Disease:
- Anemia
- Fatigue
- Nausea
- Joint pain
- Thinning hair (and high forehead)
- Dull skin complexion
- Skin Rashes
- Gas and bloating
Non-Celiac Gluten Sensitivity
Unlike an allergy, non-celiac gluten sensitivity is a non-IgE immune response. And that would be IgM, IgG, or IgA. Remember, there are different branches of the armed forces. Your immune system is like the armed forces. It’s there to protect you. You have an Army, an Air Force, Marines, Coast Guard. IgA, IgG, IgE, IgM. So this category is non-IgE immune response. There is a tremendous amount of discussion in the literature about this category. This includes the world of non-celiac gluten sensitivity.
Most of its symptoms occur outside of the intestines and gastrointestinal tract. People with gluten sensitivity develop symptoms after eating gluten, but the immune reaction is different than the one that occurs in celiac disease. non-celiac gluten sensitivity is more common than celiac disease.
In one study, researchers from Italian medical centers that specialize in the diagnosis and treatment of gluten-related disorders identified nearly 500 patients with suspected non-celiac gluten sensitivity. They used patients’ reported symptoms, lab tests, intestinal biopsy results (if performed), and other factors to identify those who were sensitive to gluten.
The most common symptoms reported in people with gluten sensitivity included:
- Bloating (87%)
- Abdominal pain (83%)
- Lack of well being (68%)
- Tiredness (64%)
- Headache (54%)
- Diarrhea (54%)
- Nausea (44%)
- Anxiety (39%)
- Brain fog (38%)
- Numbness (32%)
- GERD (32%)
- Joint/muscle pain (31%)
Gluten-sensitive people in the study also experienced constipation, rashes, weight loss, anemia, depression, mouth sores, and more. More women than men suffered from gluten sensitivity, by a ratio of more than 5 to 1. The average age of the patients was 38. Nearly half of the patients had irritable bowel syndrome (IBS) while 35% reported food intolerance. Almost 1 in 5 patients had a relative with celiac disease. Researchers reported that 14% of gluten-sensitive people in the study had an autoimmune disease, most commonly autoimmune thyroiditis.
Non-immune Malabsorption Syndrome
Your body is opportunistic, seeking to draw in and utilize as many nutrients as it can. When you ingest foods, the expectation is that your body can and will use whatever properties that food provides, and discard as waste that which it cannot. But if you have a malabsorption syndrome, foods go through you without reaping much benefit.
There are different tests that may indicate a problem, such as high fat content in the stools. The tests chosen greatly depend upon symptoms, medical history, and the suspected reason behind your malabsorption syndrome.
Common Symptoms of Malabsorption Syndrome
- Frequent diarrhea
- Floating stools
- Foul smelling stools
- Weight loss
- Difficulty gaining weight
- Addressing Gluten-Related Disorders
- Avoid gluten.
The #1 rule for addressing gluten-related disorders is to avoid gluten. This includes inhaling it, eating it, putting it on your skin or hair. Wherever your body finds it, it will attack if you have a problem with gluten (or wheat).
Hidden gluten is EVERYWHERE.
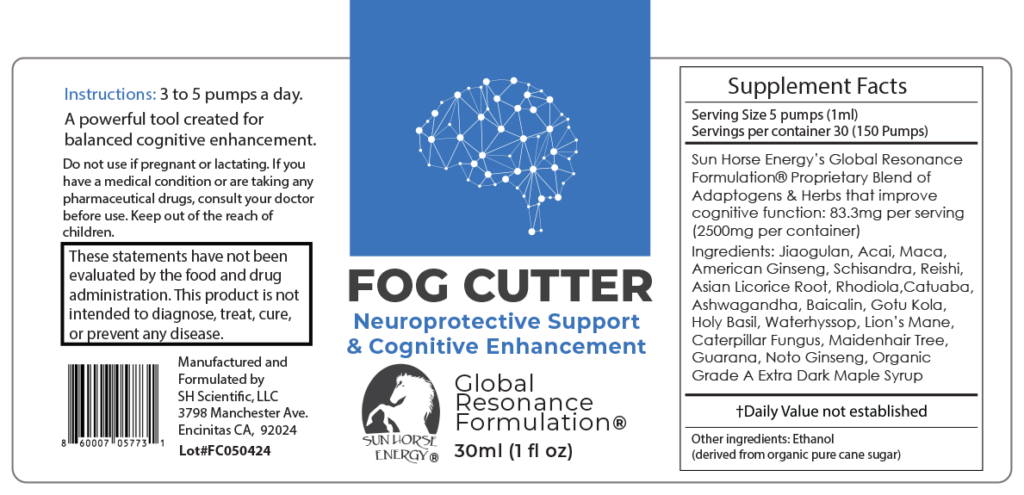
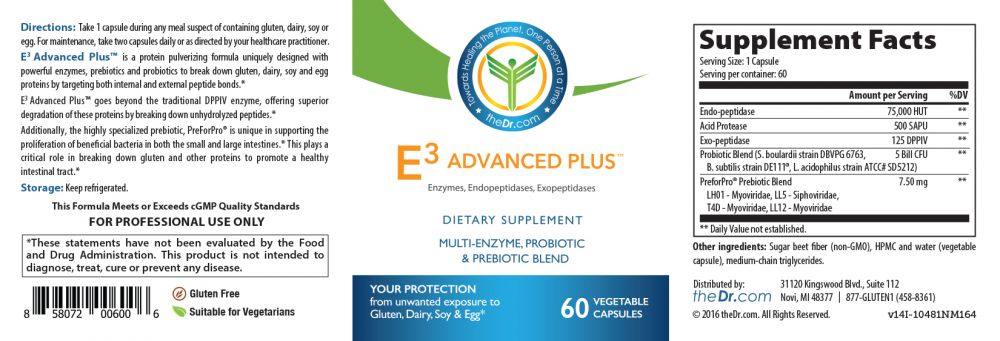
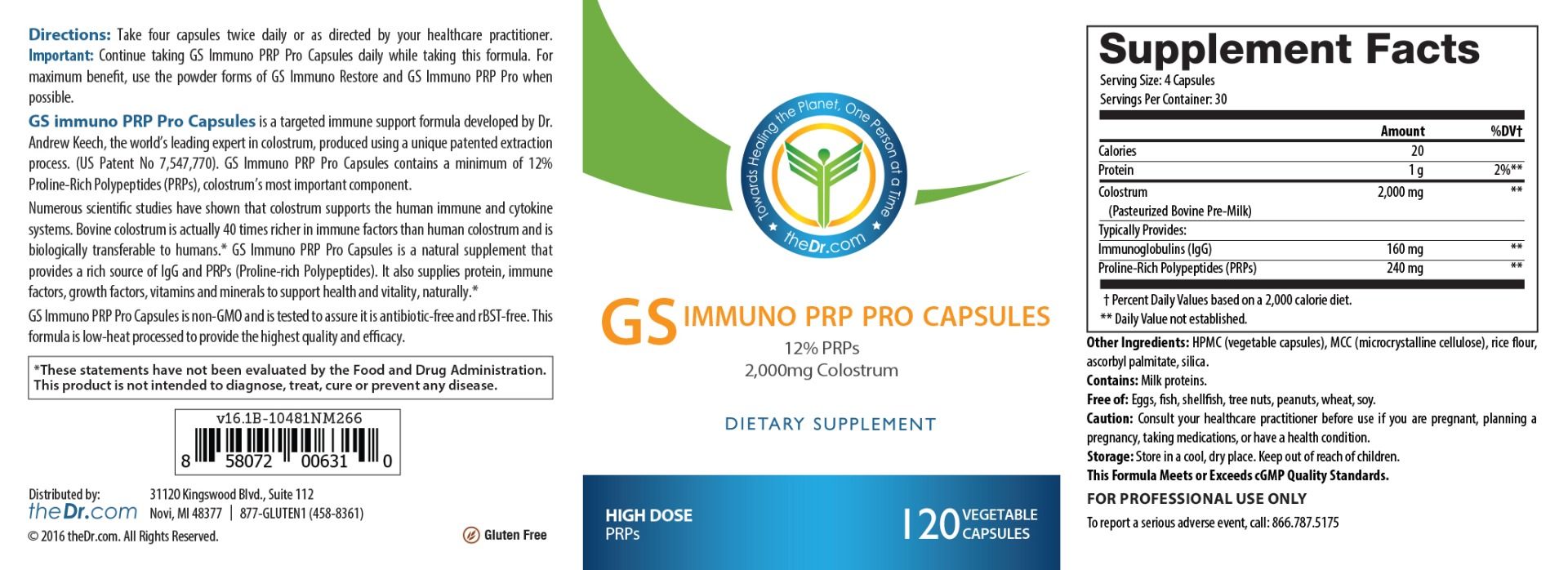
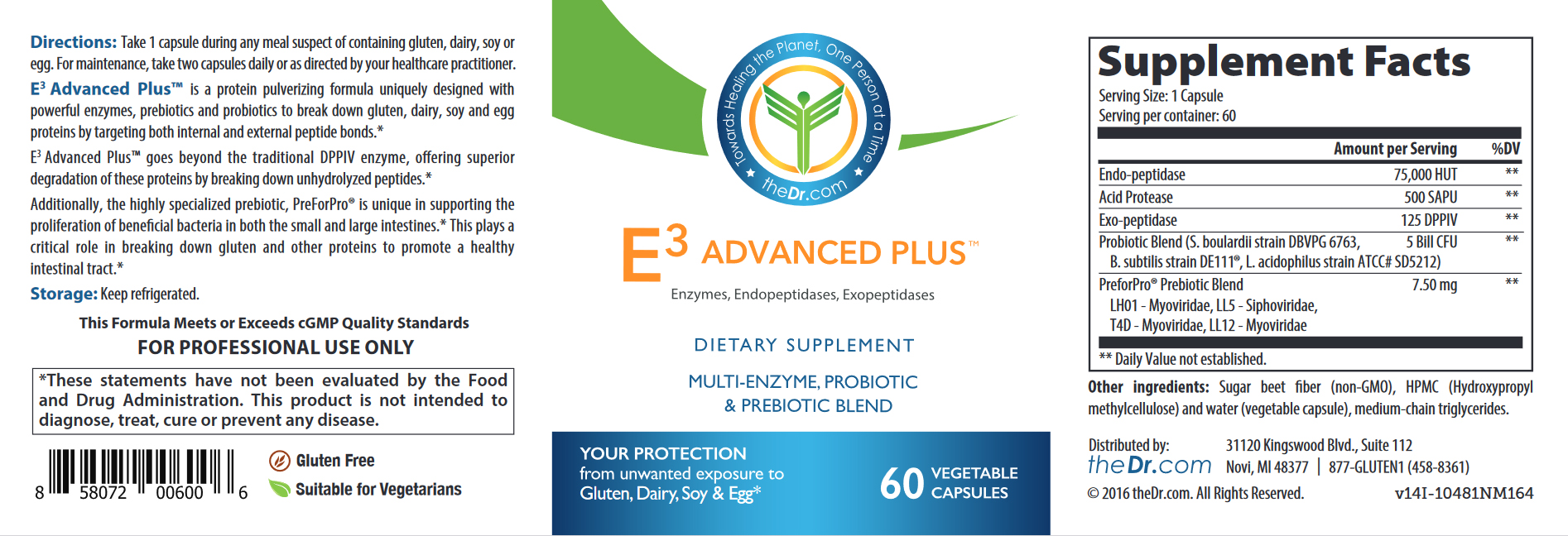
It isn’t just in your food, so learn what to look for and where your most likely accidental exposures may happen. To address cross-contamination preventatively in high-risk situations like eating out, take E3 Advanced Plus or WheatRescue. Both of these products act to breakdown gluten proteins within 90 minutes (prior to entry into the small intestine where the autoimmune response occurs).
Know when to seek emergency treatment.
If you have an allergy to wheat or gluten, carry an EpiPen in case of an extreme reaction like anaphylaxis. This can be a dangerous and life threatening situation if left untreated. Some signs include constriction of air pathways making it difficult to breathe, a weak and rapid heartbeat, fainting, dizziness, hives, and nausea. This requires an immediate trip to the emergency room — even after you have injected yourself with epinephrine and begun showing improvement. You can have a second reaction called biphasic anaphylaxis.
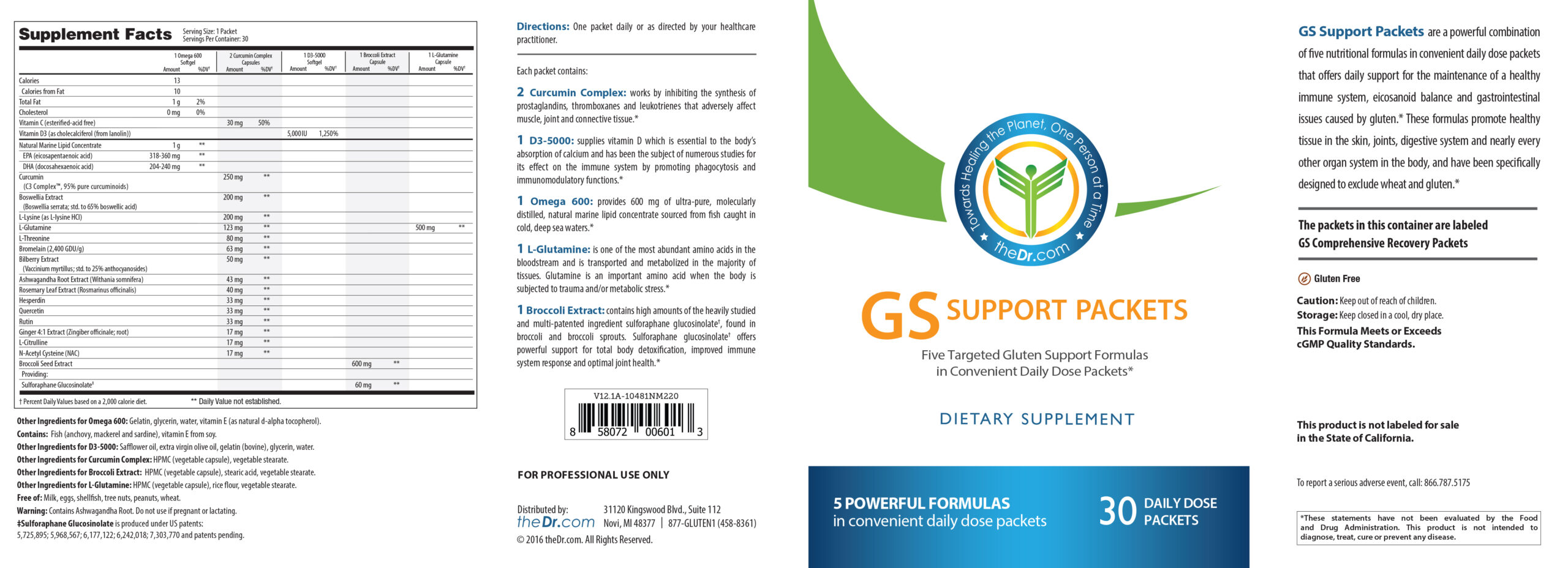
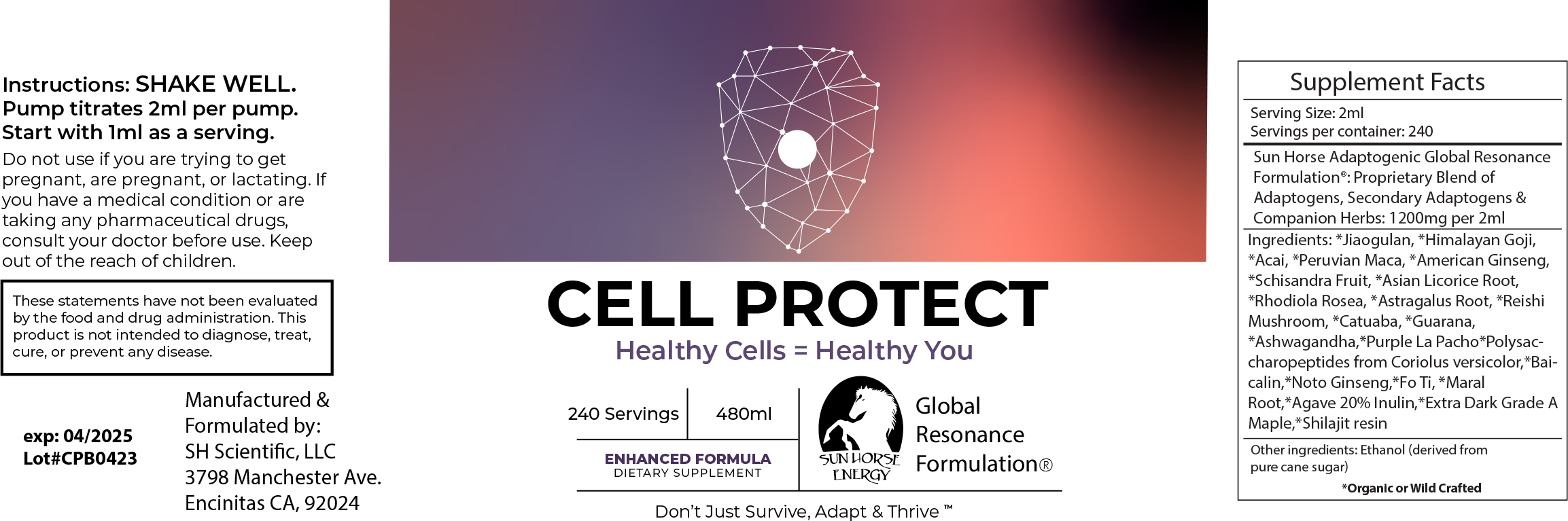
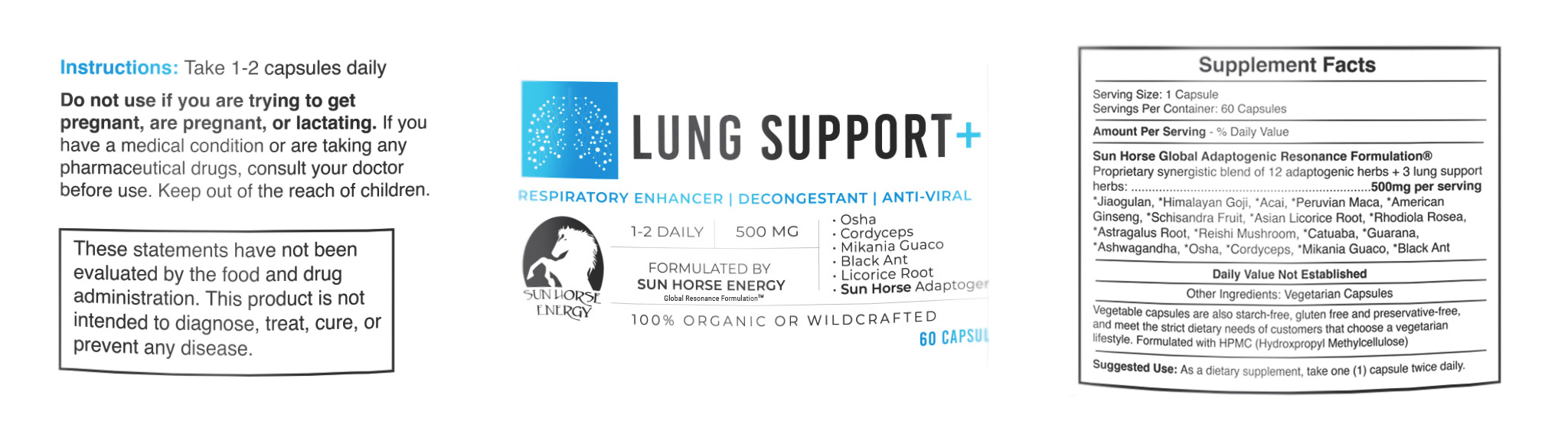
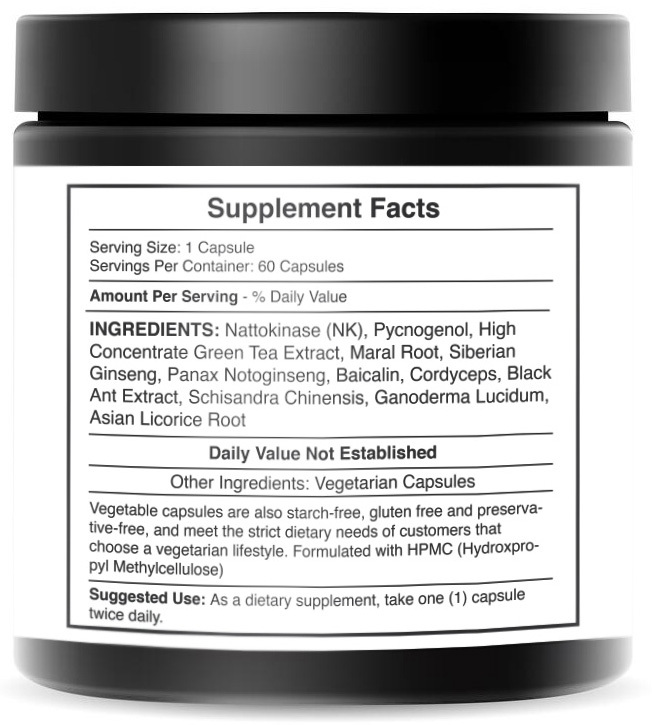
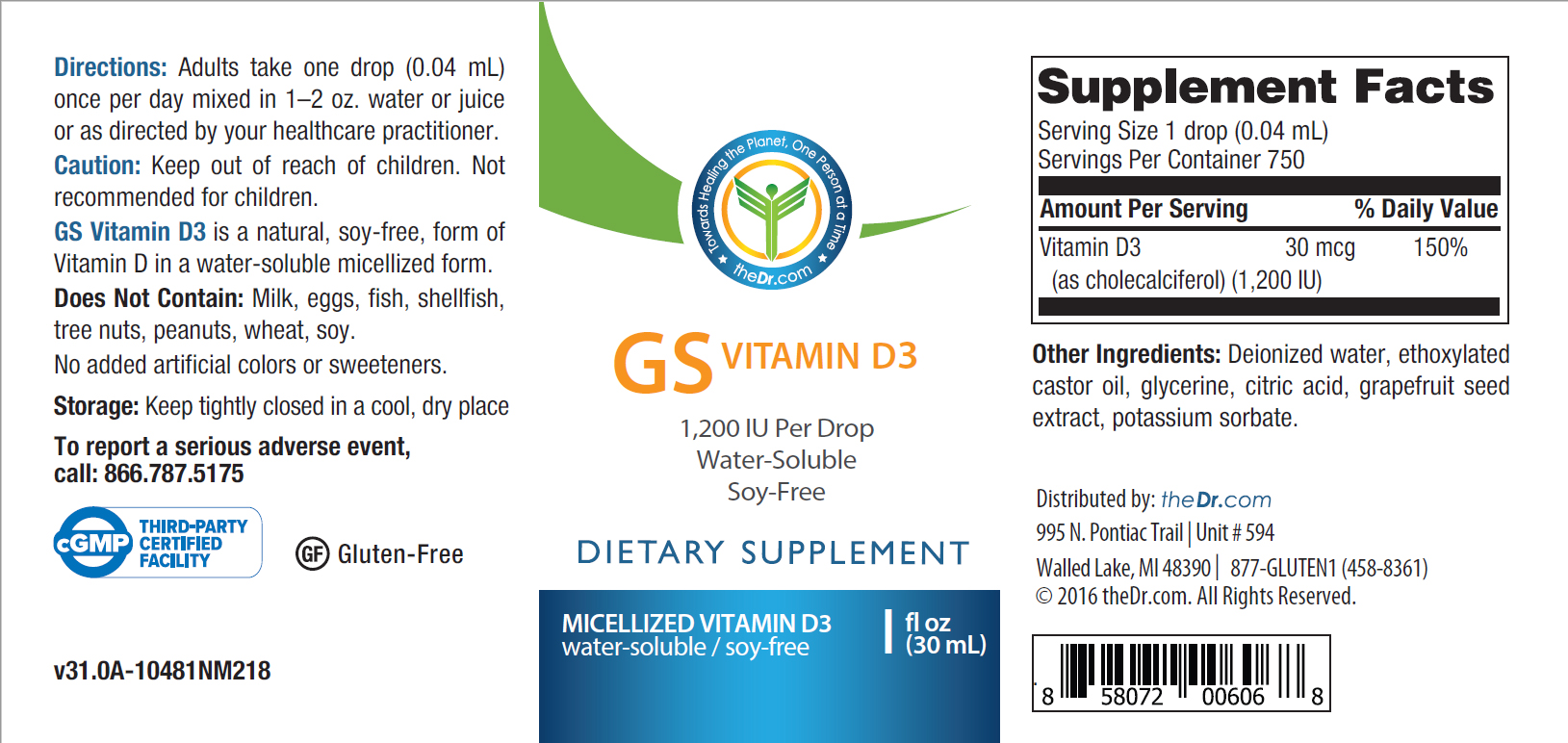
Supplement as needed
With the necessary absence of gluten in your diet, your microbiome changes and you can lose prebiotics that feed the probiotics in your gut that protect you. Other nutritional changes occur due to your change in diet. If you don’t address these changes, you could inadvertently end up causing an inflammatory cascade of events while attempting to address your gluten-related disorder. See a nutritionist who can guide you in adjusting your diet to not just exclude gluten, but to include foods that will make up for the nutritional losses.
Test periodically.
People who have been living gluten-free assume they no longer need to get tested. They tested to discover the problem, and now they are on a gluten-free diet. What’s the point? Without periodic testing, you don’t know if the protocol you are using is actually working. If you think you are gluten-free and antibodies are firing away, you may not feel it until an autoimmune disease rears its ugly head. You want to make adjustments before feeling symptoms.Tests give you insight into what’s really going on, so that you can make whatever improvements and modifications in what you are currently doing in order to be more successful.
Who wants to go through all the trouble of being on a gluten-free diet only to realize that one of their daily exposures keeps them in the same predicament as before? Test. Fix. Retest.
You Can’t Eat a Little Gluten.
When you have a gluten-related disorder, you can’t eat a little gluten every now and then. Maintaining a gluten-free diet can feel restrictive and require a commitment to your health, but your health is at risk when you eat gluten. So avoid it.
If you go to someone’s house to eat, bring a dish you can eat. Slowly educate friends and family about what you can and can’t eat — and WHY! It isn’t a fad. It’s a health condition.
Rather than dwelling in what once was, becoming increasingly isolated, or giving in on special occasions, find ways to create opportunities to be included that allow you to eat.
With time and dedication, you will get some basics down and begin to expand out into exploring new foods and finding ways that work easily within your lifestyle. Give yourself time to get used to this new way of life, and remind yourself why you are doing it in the first place. Find treats that are gluten-free that allow you to not feel denied and keep you on a path to wellness.
To find a wealth of information about gluten-related disorders, add The Gluten Summit to your health library. The Gluten Summit gathers 29 of the world’s experts for a one-to-one conversation with me about celiac disease, food sensitivities, autoimmunity, nutrition and more. Find your motivation through patient education.
Celiac disease is only one of several gluten-related disorders. A recent paradigm shift has occurred within the healthcare field with the recognition that non-celiac gluten sensitivity is at least six-fold, and (so far) as high as 20-fold more frequent than celiac disease — and there are even more gluten-related disorders where those came from.
How do we differentiate the world of gluten-related disorders? This is a critical discussion. Would you treat an IgE reaction the same as an IgA reaction? There are similarities in protocols, but each carries a different emphasis.
There is a spectrum of gluten-related disorders. Now, what does that mean? It means there are at least four different conditions that fall under the category of a “gluten-related disorder.”
Here we cover the four most recognized categories of gluten-related disorders.
Allergy (IgE)
The first one—the oldest of these in terms of being identified in medical literature—is an allergy, more specifically a wheat allergy. That’s an IgE reaction. And those tests came out in the 1950s. The skin prick test is still used today. It can be diagnosed by skin pricking or by a blood test.
Any other immunoglobulin response cannot be called an allergy because the first immune response that was identified was coined as an allergy — an IgE response.
To get your language right so that you are referring to the proper conditions when you’re talking with your peers, do not refer to a gluten-related disorder as an allergy unless there is an IgE response present. Refer to it simply as a gluten-related disorder.
Common symptoms of a wheat allergy include:
- Swelling, itching or irritation of the mouth or throat
- Hives, itchy rash or swelling of the skin
- Stuffy or runny nose
- Headaches
- Itchy, watery eyes
- Cramps, nausea or vomiting
- Diarrhea
In the following serious but rare circumstances listed below, seek emergency treatment immediately:
- Difficulty breathing
- Anaphylaxis
- Heart palpitations
Celiac Disease
Celiac disease is the most well-known gluten-related disorder. In fact, many people don’t even realize there are other gluten-related problems other than celiac disease. It’s an autoimmune condition that results in tissue damage in the small intestine. Celiac disease is unique and separate in its own way.
The standard test for celiac disease looks at transglutaminase antibodies [IgA transglutaminase antibodies]. There are nine different transglutaminases. We look at transglutaminase 2, which is on the microvilli in the intestines. It also covers the organs, liver, kidneys, heart, and spleen.
This test is considered the diagnostic marker for celiac disease, but there’s a problem with the test. It shows transglutaminase ninety-seven percent sensitive to identify celiac disease.
The problem is that the researchers use celiac patients in these studies, and to qualify as a celiac patient, you have total villous atrophy. In order to get diagnosed, a patient would have had an endoscopy where a doctor could see that the microvilli were worn down completely. So, if you have total villous atrophy, the transglutaminase blood test will be accurate 9.5 to 9.9 out of 10 times.
But, if you have partial villous atrophy, the test may come back negative — that’s a problem. You won’t see it in that blood test because it’s only sensitive at total villous atrophy.
I would personally like to change how the medical community views and tests for celiac disease. Rather than wait until you have reached the final stage, I propose we look at it as a spectrum so people can identify the problem early on and follow a gluten-free protocol.
We already have the ability to do this. In the US, we have an excellent tool to distinguish between celiac, non-celiac gluten sensitivity, non-gluten wheat sensitivity and autoimmune processes triggered by gluten: the Vibrant Wellness Wheat Zoomer test. At this time, it is available everywhere in the US except New York.
In both the US and internationally, we have the Cyrex Array Panels.
Unless you notice an immediate reaction upon eating a food, it can be difficult to make the association between the food and symptoms that can appear later. Many people with celiac experience problems outside of their gut, making it even less likely to make a food association.
Some Common Symptoms of Celiac Disease:
- Anemia
- Fatigue
- Nausea
- Joint pain
- Thinning hair (and high forehead)
- Dull skin complexion
- Skin Rashes
- Gas and bloating
Non-Celiac Gluten Sensitivity
Unlike an allergy, non-celiac gluten sensitivity is a non-IgE immune response. And that would be IgM, IgG, or IgA. Remember, there are different branches of the armed forces. Your immune system is like the armed forces. It’s there to protect you. You have an Army, an Air Force, Marines, Coast Guard. IgA, IgG, IgE, IgM. So this category is non-IgE immune response. There is a tremendous amount of discussion in the literature about this category. This includes the world of non-celiac gluten sensitivity.
Most of its symptoms occur outside of the intestines and gastrointestinal tract. People with gluten sensitivity develop symptoms after eating gluten, but the immune reaction is different than the one that occurs in celiac disease. non-celiac gluten sensitivity is more common than celiac disease.
In one study, researchers from Italian medical centers that specialize in the diagnosis and treatment of gluten-related disorders identified nearly 500 patients with suspected non-celiac gluten sensitivity. They used patients’ reported symptoms, lab tests, intestinal biopsy results (if performed), and other factors to identify those who were sensitive to gluten.
The most common symptoms reported in people with gluten sensitivity included:
- Bloating (87%)
- Abdominal pain (83%)
- Lack of well being (68%)
- Tiredness (64%)
- Headache (54%)
- Diarrhea (54%)
- Nausea (44%)
- Anxiety (39%)
- Brain fog (38%)
- Numbness (32%)
- GERD (32%)
- Joint/muscle pain (31%)
Gluten-sensitive people in the study also experienced constipation, rashes, weight loss, anemia, depression, mouth sores, and more. More women than men suffered from gluten sensitivity, by a ratio of more than 5 to 1. The average age of the patients was 38. Nearly half of the patients had irritable bowel syndrome (IBS) while 35% reported food intolerance. Almost 1 in 5 patients had a relative with celiac disease. Researchers reported that 14% of gluten-sensitive people in the study had an autoimmune disease, most commonly autoimmune thyroiditis.
Non-immune Malabsorption Syndrome
Your body is opportunistic, seeking to draw in and utilize as many nutrients as it can. When you ingest foods, the expectation is that your body can and will use whatever properties that food provides, and discard as waste that which it cannot. But if you have a malabsorption syndrome, foods go through you without reaping much benefit.
There are different tests that may indicate a problem, such as high fat content in the stools. The tests chosen greatly depend upon symptoms, medical history, and the suspected reason behind your malabsorption syndrome.
Common Symptoms of Malabsorption Syndrome
- Frequent diarrhea
- Floating stools
- Foul smelling stools
- Weight loss
- Difficulty gaining weight
- Addressing Gluten-Related Disorders
- Avoid gluten.
The #1 rule for addressing gluten-related disorders is to avoid gluten. This includes inhaling it, eating it, putting it on your skin or hair. Wherever your body finds it, it will attack if you have a problem with gluten (or wheat).
Hidden gluten is EVERYWHERE.
It isn’t just in your food, so learn what to look for and where your most likely accidental exposures may happen. To address cross-contamination preventatively in high-risk situations like eating out, take E3 Advanced Plus or WheatRescue. Both of these products act to breakdown gluten proteins within 90 minutes (prior to entry into the small intestine where the autoimmune response occurs).
Know when to seek emergency treatment.
If you have an allergy to wheat or gluten, carry an EpiPen in case of an extreme reaction like anaphylaxis. This can be a dangerous and life threatening situation if left untreated. Some signs include constriction of air pathways making it difficult to breathe, a weak and rapid heartbeat, fainting, dizziness, hives, and nausea. This requires an immediate trip to the emergency room — even after you have injected yourself with epinephrine and begun showing improvement. You can have a second reaction called biphasic anaphylaxis.
Supplement as needed
With the necessary absence of gluten in your diet, your microbiome changes and you can lose prebiotics that feed the probiotics in your gut that protect you. Other nutritional changes occur due to your change in diet. If you don’t address these changes, you could inadvertently end up causing an inflammatory cascade of events while attempting to address your gluten-related disorder. See a nutritionist who can guide you in adjusting your diet to not just exclude gluten, but to include foods that will make up for the nutritional losses.
Test periodically.
People who have been living gluten-free assume they no longer need to get tested. They tested to discover the problem, and now they are on a gluten-free diet. What’s the point? Without periodic testing, you don’t know if the protocol you are using is actually working. If you think you are gluten-free and antibodies are firing away, you may not feel it until an autoimmune disease rears its ugly head. You want to make adjustments before feeling symptoms.Tests give you insight into what’s really going on, so that you can make whatever improvements and modifications in what you are currently doing in order to be more successful.
Who wants to go through all the trouble of being on a gluten-free diet only to realize that one of their daily exposures keeps them in the same predicament as before? Test. Fix. Retest.
You Can’t Eat a Little Gluten.
When you have a gluten-related disorder, you can’t eat a little gluten every now and then. Maintaining a gluten-free diet can feel restrictive and require a commitment to your health, but your health is at risk when you eat gluten. So avoid it.
If you go to someone’s house to eat, bring a dish you can eat. Slowly educate friends and family about what you can and can’t eat — and WHY! It isn’t a fad. It’s a health condition.
Rather than dwelling in what once was, becoming increasingly isolated, or giving in on special occasions, find ways to create opportunities to be included that allow you to eat.
With time and dedication, you will get some basics down and begin to expand out into exploring new foods and finding ways that work easily within your lifestyle. Give yourself time to get used to this new way of life, and remind yourself why you are doing it in the first place. Find treats that are gluten-free that allow you to not feel denied and keep you on a path to wellness.
To find a wealth of information about gluten-related disorders, add The Gluten Summit to your health library. The Gluten Summit gathers 29 of the world’s experts for a one-to-one conversation with me about celiac disease, food sensitivities, autoimmunity, nutrition and more. Find your motivation through patient education.