Eating Gluten During Pregnancy May Raise Your Child’s Risk of Adult Schizophrenia
Think whole wheat makes for a healthy pregnancy? If so, think again. According to one study, gluten sensitivity may more than double your child’s risk of developing schizophrenia later in life.
You may have noticed an increasing number of gluten-free items popping up on grocery store shelves and more restaurants offering gluten-free options. Awareness is growing as rates of celiac disease, an intestinal autoimmune disease caused by gluten, has quadrupled in the last 50 years. The numbers could be much higher; it’s estimated that 95 percent of those with celiac disease go undiagnosed.
Researchers also estimate the numbers of people with gluten sensitivity—a non-celiac inflammatory reaction to gluten—is approximately 30 percent of the population.
Gluten refers to the proteins found in wheat, spelt, rye, barley, kamut, and triticale. It can also be found in foods that don’t normally contain gluten but have been cross-contaminated with foods containing gluten. For instance, grains such as oats may share the same facilities used by foods that naturally contain gluten, like wheat. Contamination occurs when foods like oats make contact with the dust of the flours. This is common, so unless something clearly states “gluten-free,” it may be suspect.
The onset of schizophrenia usually occurs in late adolescence to early adulthood, between 16 and 30 years old. It is characterized by an individual’s inability to differentiate between reality and their own perceptions.
Symptoms of schizophrenia include delusions, hallucinations, and incoherent or disorganized thoughts in the absence of drugs or other health conditions. A patient may have diminished emotional responses, appearing apathetic or having a flat affect in tone and/or expression. It may also include periods of being in a catatonic state. As in life, severity and range of symptoms vary from person to person.
Gluten Sensitivity Can Cause Schizophrenia and Other Brain Disorders.
Studies have shown gluten sensitivity destroys brain and nervous tissue more than any other tissue in the body and is linked to a number of other neurological disorders. Everything from mood disorders to epilepsy to autism have been linked to gluten sensitivity. Schizophrenia is among its victims.
Back in World War II, consumption of wheat was down, and coincidentally so were hospital admissions for schizophrenia. A couple years after the war ended, the number of cases of schizophrenia rose dramatically, with an astounding and noticeable increase from one out of 30,000 people to one in 100. This happened at the same time Western grains were reintroduced into the diet. Since then, research has been done to determine if or what the relationship is between wheat and schizophrenia. It looks like it was not a coincidence.
One study analyzed blood samples of almost 800 subjects born in Sweden between 1975 and 1985. Researchers found that, compared to their peers, subjects with schizophrenia had high levels of gluten antibodies in their blood at birth, suggesting a gluten sensitivity passed to them from their mothers.
A mother’s immune antibodies pass through the placenta to the fetus to prepare it for life outside the womb. However, she also passes on immune abnormalities, such as food sensitivities, inflammation, and autoimmunity, a condition in which the immune system attacks the body. These immune imbalances profoundly impact fetal brain development.
This helps explain why infections and inflammatory disorders during pregnancy are linked to a greater risk for psychosis, autism, and other brain disorders in the offspring, although this is the first study that points to food sensitivity as a culprit.
TG6 – Your Body Betrays Your Brain
When you get a blood test to determine whether you have celiac disease, one of the markers they look for is that you are producing antibodies to transglutaminase 2 (TG2). Antibodies to TG2 can cross react with TG3 and TG6.
TG6 is the primary component of the brain. When someone eats wheat and it triggers a production of antibodies to TG6, you get inflammation in the brain. This is the most commonly identified mechanism behind a sensitivity to wheat creating symptoms in the brain.
These elevated levels signify that your immune system is attacking your brain. You have a blood-brain barrier to protect the brain from attacks; if antibodies are being produced in the brain, that means that there is likely a breach in the blood-brain barrier.
Gliadin and Schizophrenia
Gluten describes a variety of proteins. Two main groups of proteins found in gluten are gliadins and glutenins. When people refer to the word “gluten,” they are typically referring to the gluten found in wheat, barley, and rye. It is a different form of gluten than that found in other grains.
For instance, oats contain gluten, but they do not contain gliadin. Some people who are gluten-sensitive may have trouble with oats and other grains, and other people only have trouble with the gluten found in wheat, barley and rye. “Gluten” for lay people is this.
When people have an immune response to gliadin, they produce anti-gliadin antibodies.
According to a published report, Neurologic and Psychiatric Manifestations of Celiac Disease and Gluten Sensitivity, anti-gliadin antibodies are significantly higher in people with schizophrenia than in the general population.
As many as 57% of people with neurological dysfunction of unknown origin test positive for anti-gliadin antibodies. The most common peptide of wheat that the immune system fights is called alpha-gliadin, which is a signature of 33 amino acids.
Why pregnant women need to know about gluten sensitivity
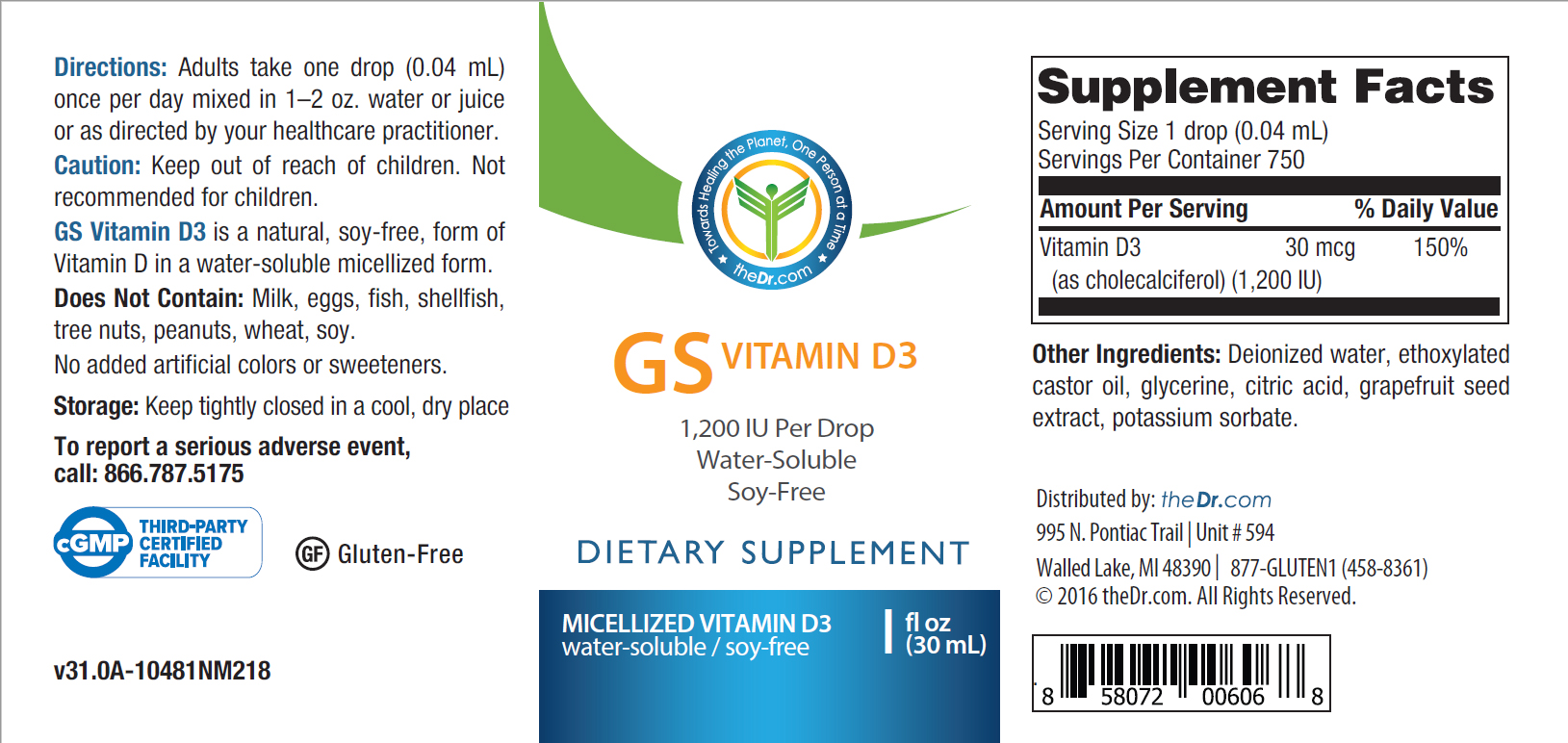
Screening for celiac disease may be recommended due to its association with an increased risk of miscarriages. If you already know you have a gluten-related disorder, addressing the additional nutritional needs while on a gluten-free diet can have implications for the pregnancy and the development of the baby.
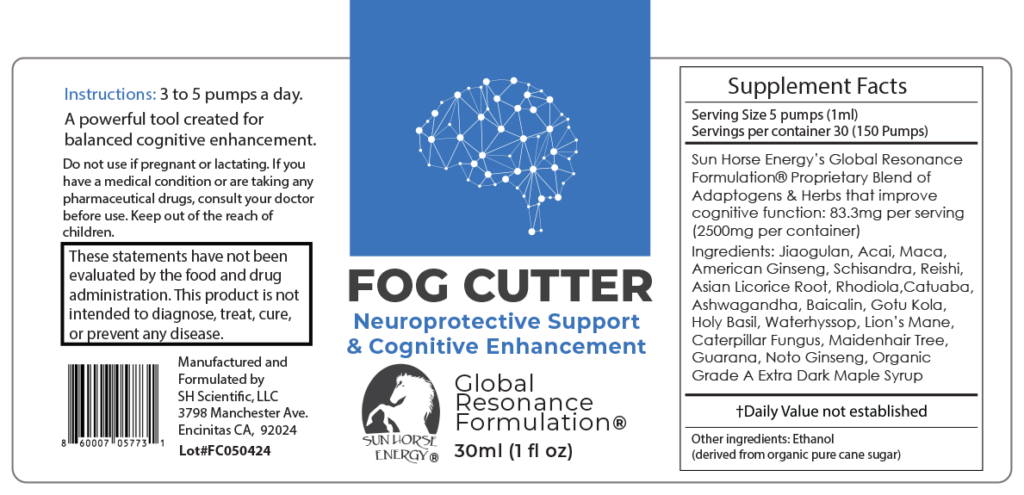
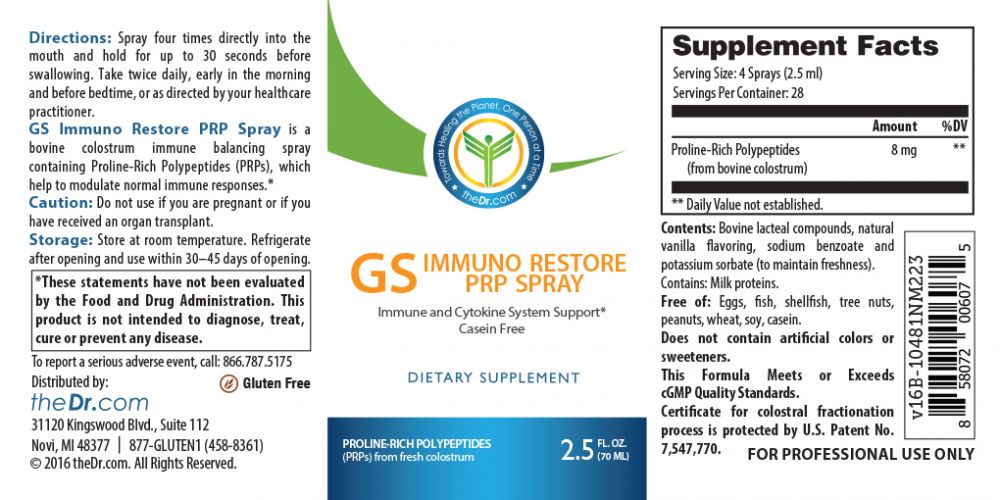
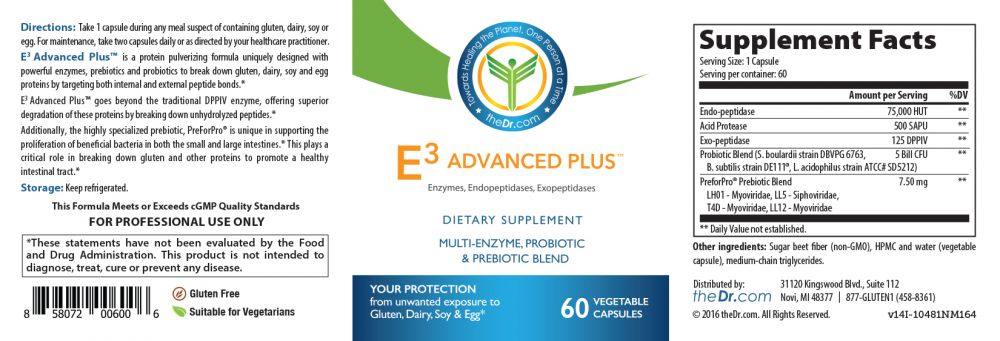
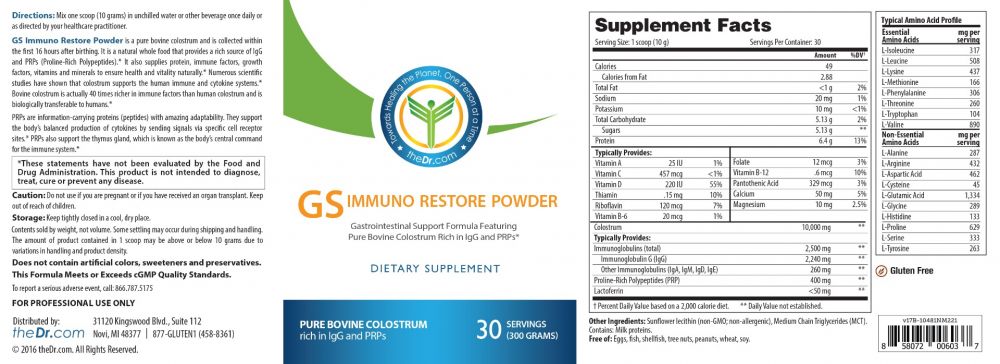
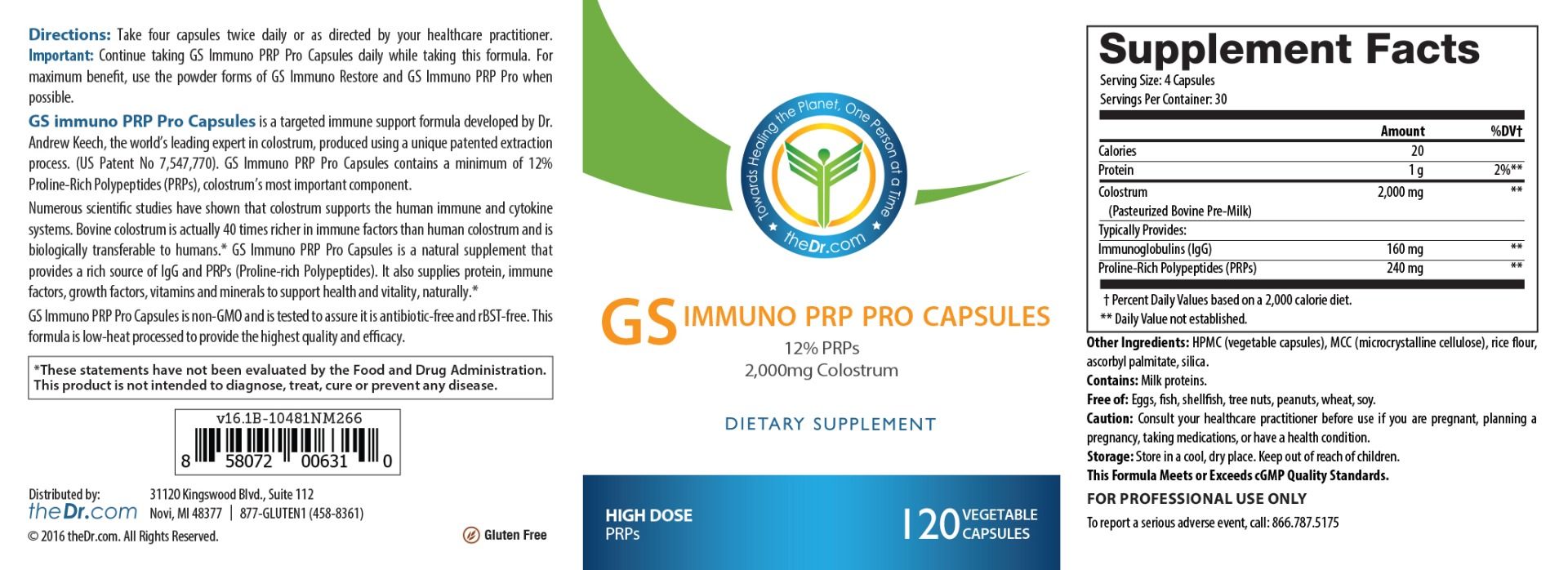
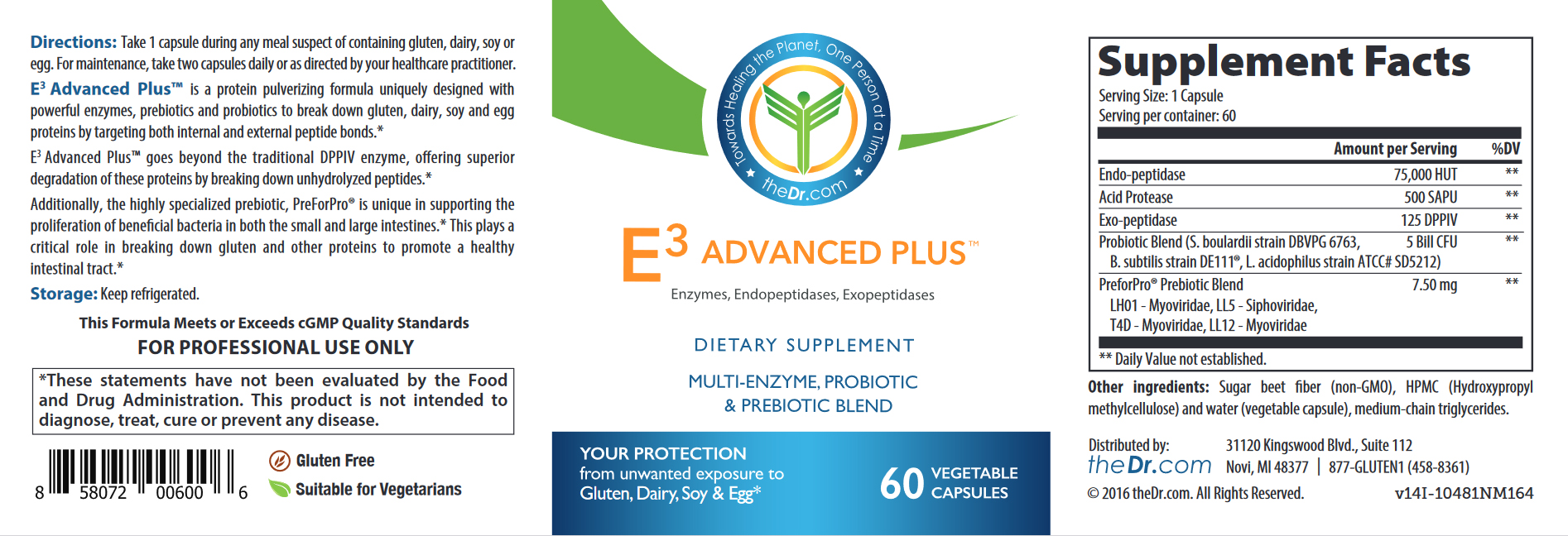
The majority of people get their probiotics (and prebiotics) through consuming wheat products. Wheat is in a lot of foods people eat, and when you remove it from your diet, you need to consider how you will address the nutritional deficits.
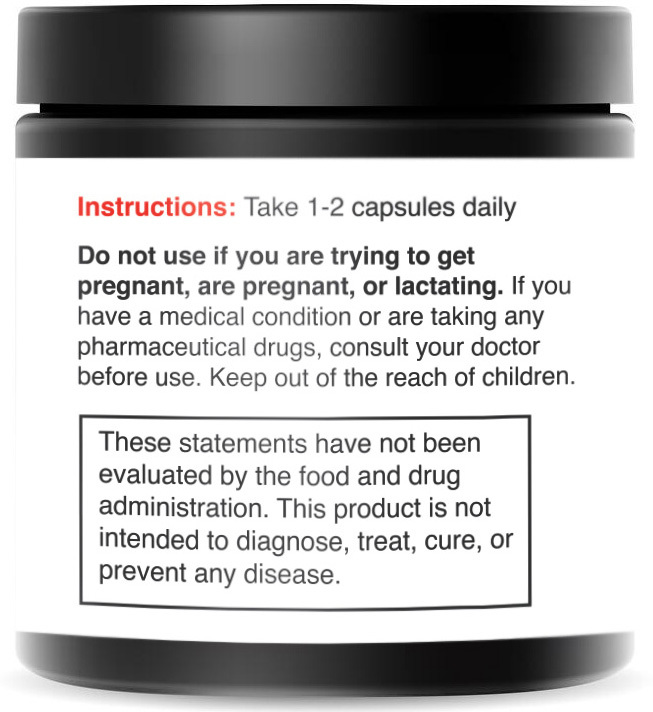
It does not mean you should eat gluten. In fact, eating gluten when it causes an autoimmune response in the mother can cause a host of problems for the developing fetus, as well as the mother-to-be. It does, however, mean you should find better alternatives to maintaining diversity and healthy gut flora.
Making changes to your diet results in changes to your microbiome, meaning it has an effect on your baby’s health, too.
How a mother’s gluten sensitivity affects her baby’s brain
Your brain has two hemispheres – the left side and the right side. Each area of the brain controls specific functions, and relies on the other side of the brain to meet appropriate developmental goals. Beginning before birth, these hemispheres develop in stages Whenever a baby or child is in early development, things can interfere with this development. This includes sickness and inflammation from a gluten sensitivity. When you throw the critical timing off, we see issues in brain development. This sets the stage for a wide range of neurological disorders such as attention-deficit/hyperactivity disorder (ADHD), autism, Tourette’s syndrome, depression, anxiety, and other childhood brain disorders. One out of five kids now has a mental disorder, and the statistics continue to rise.
If you look at the current explosion in inflammatory disorders today, the rise of these brain-based disorders is less of a mystery. Immune-activated mothers are giving birth to immune-activated babies.
Why Every Woman Needs to Consider a Screen for Gluten Sensitivity
All pregnant women and all women who want to have babies, should be checked for anti-gliadin antibodies, and if that test comes back positive, go on a gluten-free diet before pregnancy. We don’t know at which point during pregnancy a mother’s gluten sensitivity impacts the fetal brain, but we do know the baby’s brain and nervous system begin developing in the first trimester. Although the association between a mother’s gluten sensitivity and the baby’s increased risk of psychosis as an adult is not yet fully understood, it makes sense to go on a gluten-free diet.
It is important to note that being free of gut symptoms doesn’t necessarily mean you’re in the clear, as everyone reacts differently to gluten sensitivity. Symptoms can appear anywhere in the body, not just the gut. In fact, research suggests the majority of people with gluten sensitivity have no gastrointestinal symptoms whatsoever. For every person with gut symptoms caused by gluten, there will be eight who have none.
Gluten Sensitivity Is Not A Guarantee of Schizophrenia and Other Brain Disorders.
Undiagnosed gluten sensitivity or celiac disease in pregnancy in no way guarantees your child will develop schizophrenia or other brain disorders. “This is an association,” says one study’s lead investigator Håkan Karlsson, M.D. Ph.D., a neuroscientist at Karolinska Institutet and former neuro-virology fellow at Johns Hopkins. “We do not know if there is a causal relation between maternal anti-gluten antibodies and psychosis in the offspring. However, many women — and men — may be better off on a gluten-free diet even though they do not have celiac disease.”
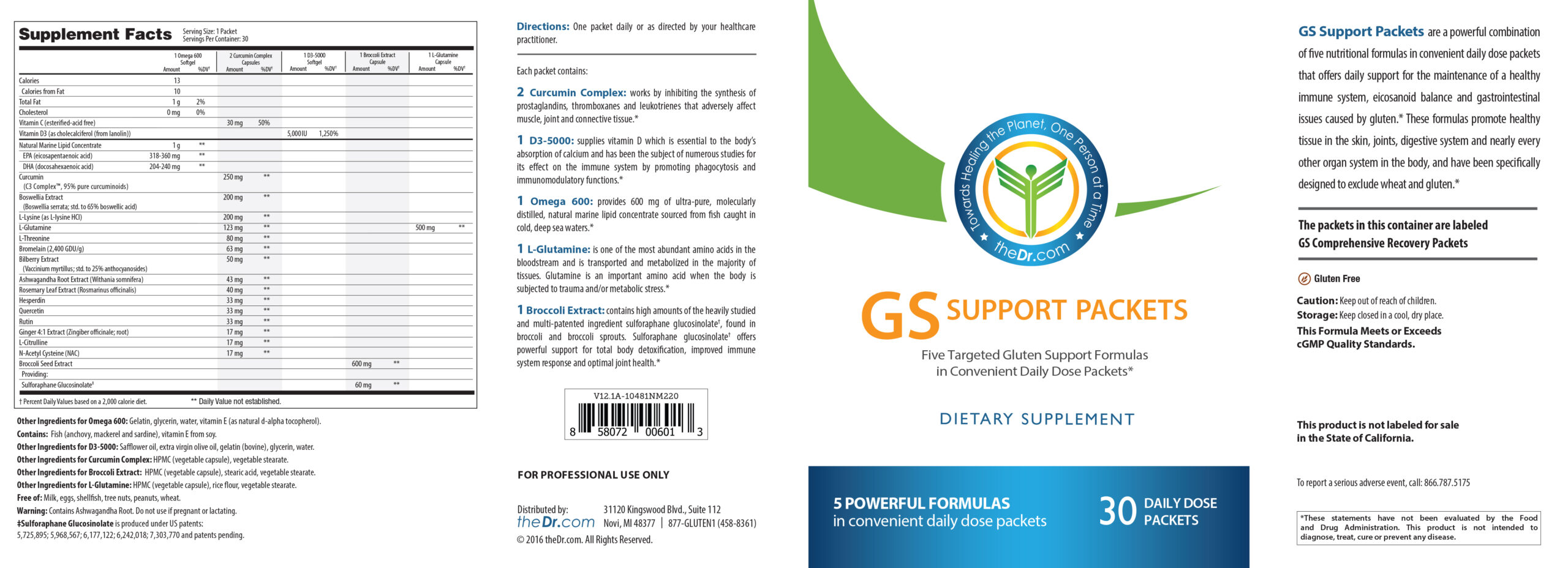
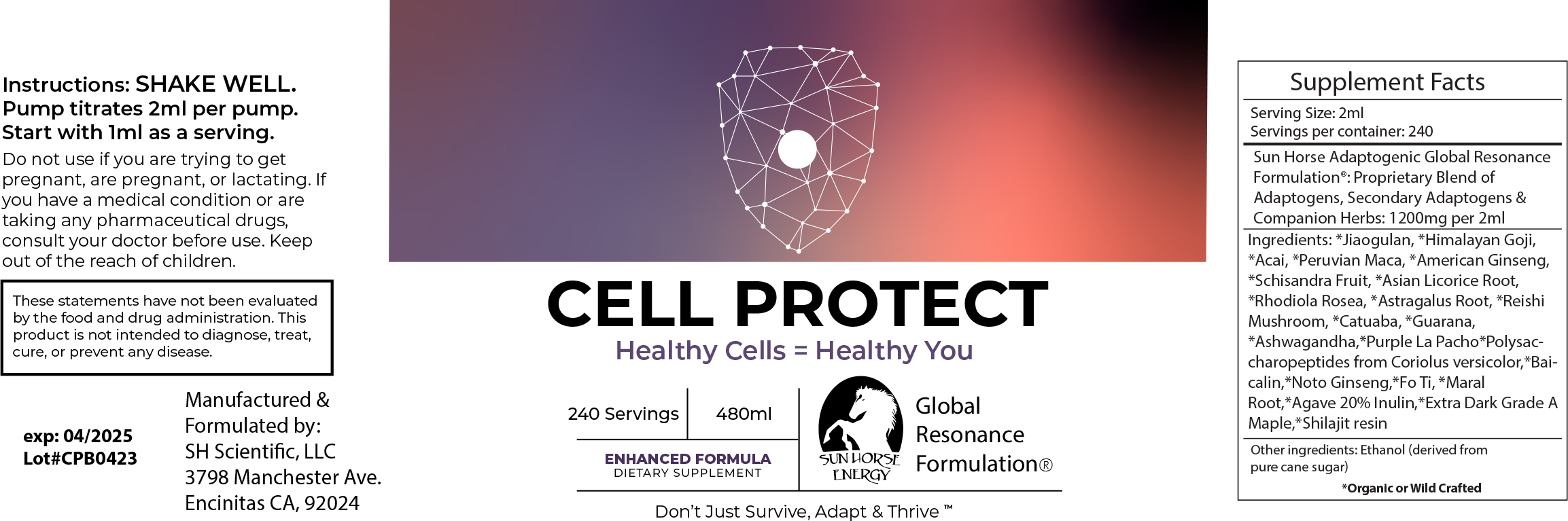
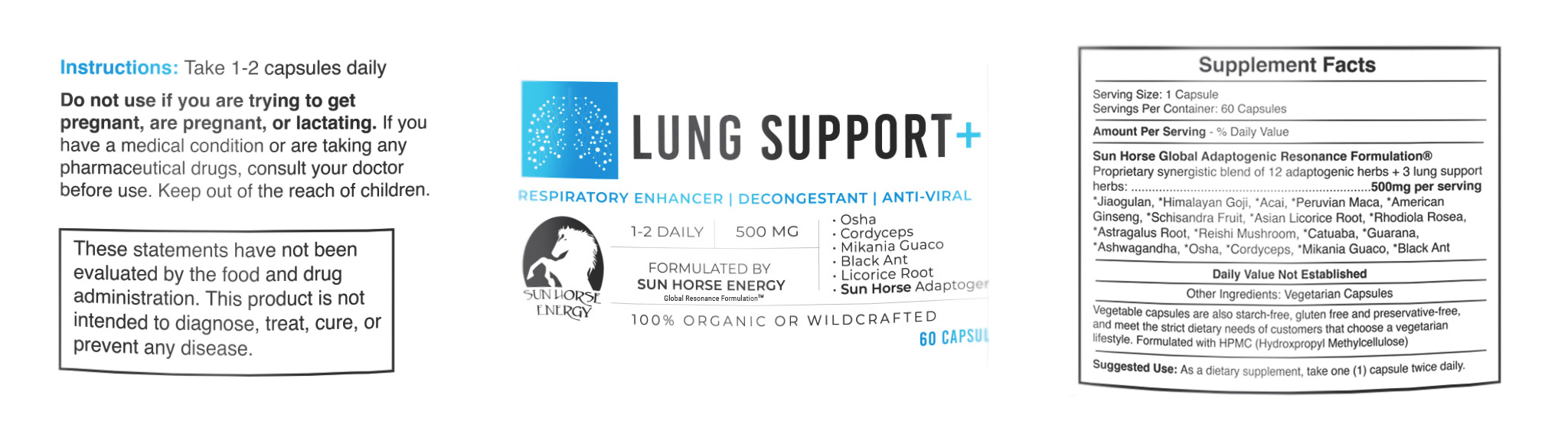
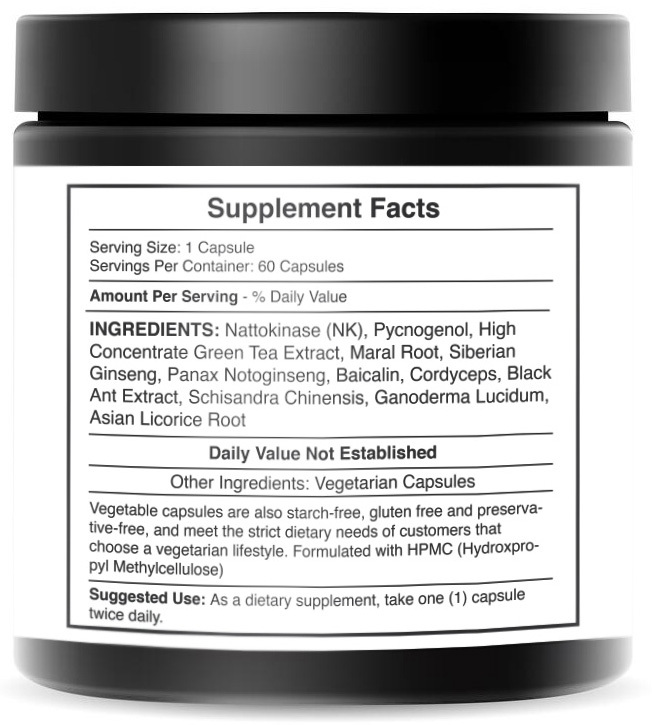
Foods are common triggers that are often overlooked in both prevention and treatment. No one food is a single trigger. However, when we see certain foods routinely cause inflammation and trigger immune responses, we can look at patterns of disease. Here, there is a clear association and a simple solution — a gluten-free diet.
Evidence indicates great promise in treatment for schizophrenia with a gluten-free diet for people with schizophrenia who test positive for antibodies to gluten. Case studies have shown improvement and even elimination of symptoms to the extent that patients were able to go off of antipsychotic medications simply by changing their diet. Food can be medicine, or it can be poison. Every person is different.
If you have schizophrenia and you are not producing these antibodies to gluten, however, the jury is still out on whether or not it will help with your symptoms related to schizophrenia. You can easily test this by going on a gluten-free diet and seeing if your own symptoms improve. Just remember to add in those probiotics and prebiotics to adjust for the change in your diet.
Another point should be made for anyone who tests positive for antibodies to gluten. Whether or not you have schizophrenia, if you are producing antibodies to gluten, you need to immediately stop eating gluten. You are hurting yourself every time you eat so much as even an eighth of the size of your fingernail of gluten. Your body is fighting to keep you alive, so it continues pumping out those antibodies for months to make sure it gets rid of this foreign invader. To you, gluten is a toxin. That toxin could lead to multiple autoimmune conditions that could ultimately be the death of you.
If that sounds alarmist, it should be your alarm to stop the path you are currently on and reroute to a better destination. Remember: you are not alone. TheDr has a ton of support to help you on your journey to make navigating a little easier.